Menu
The dentistry profession has been altered by the recent COVID-19 crisis The virus triggers inflammatory responses and respiratory distress interactions. It can kill those people with higher levels of pre-existing systemic inflammation and those who are immunocompromised. Everyone is now alert to the danger and there is a rising need to keep vulnerable people safe for the present and long-term future.
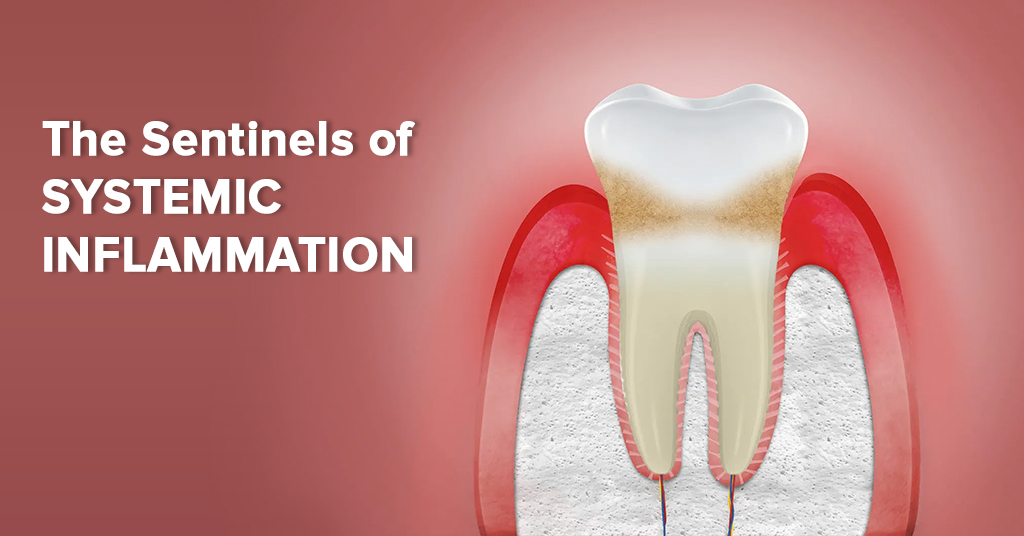
The health model of dental patients should be analysed and improved by dental professionals. If we can help reduce conditions that are linked with systemic inflammation, such as atherosclerosis and accelerated aging, then we could ensure a safer future. We could act as the “sentinels of systemic inflammation” to tackle this crisis headon!
THE DANGERS OF INFLAMMATION IN AN ORAL CONTEXT
“Systemic inflammation is the number one factor in atherosclerosis and accelerated aging,” wrote Drs. Brad Bale and Amy Doneen, famous cardiovascular specialists and authors of Beat the Heart Attack Gene. They also highlighted the part inflammation plays in peripheral microvascular diseases, and in other conditions varying as widely as between wrinkles to dementia. Patients and clients need to be encouraged to pursue an anti-inflammatory lifestyle to stay safe in a world full of virii. We are oral medicine specialists. It is our role to deconstruct the connection between oral and systemic inflammation and to explain it to our communities.
There are three main oral-systemic inflammatory connections:
There are two major issues that bacterial pathogens are responsible for, with local and systemic implications:
Research shows that when plaque-clogged arteries are put under microscopic examination after cleaning out (carotid endarterectomies), oral periodontal pathogens are commonly found in the plaque. Periodontal tissue often has high-risk oral pathogens: Aa, Fn, Pg, Td, and Tf stimulate monocytes, macrophages, foam cells, neutrophils, cytokines, MMPs, and prostaglandins due to the body’s inflammatory responses. This inflammatory cascade is popularly known as periodontal disease. The risk of unstable atherosclerosis would be increased through an inflammatory cascade from a similar response in the arterial lining that occurs in the lining of teeth.
Furthermore, other research has shown that a considerable number of heart attack patients were found to have periapical pathogens (Streptococcus) in 78% of their obstructing thrombi (clots). This entails that oral bacteria and dental infections are linked to the development of certain heart attacks (i.e. acute coronary thrombosis). Dental health needs to be a crucial element in the process of avoiding heart attacks.
Dental professionals need to be the sentinels of systemic inflammation, responsible for preventing high-risk oral pathogens from damaging the health of the mouth and the body. We will advance in the battle to eradicate these inflammatory agents through testing, education, and implementation.
Oxygen is an essential mover of physiological processes. When it depletes within the bloodstream, an inflammatory cascade quickly follows. Blood pressure and heart rate increases due to the cortisol released from the adrenals, off a “fight-or-flight” response. These chronic oxygen desaturations can gradually mislead the human body to heart attacks, insulin resistance, sleep disturbances, cardiac arrhythmia, diabetes, memory loss, and strokes. These conditions emerge from the onset of childhood through sleep apnea, nasal allergies, nasal congestion, obstructed airways, swollen tonsils and adenoids, snoring, and ADHD-like behavior.
Dental malocclusions imply breathing and sleep disorders. These include and are not restricted to crossbites, maxillary vertical excess, anterior open bites, scalloping of the tongue, tongue thrust and tongue-ties, descended soft palates and uvulas, increased caries, and periodontal inflammation.
Dental professionals need to be the sentinels of systemic inflammation, responsible for preventing high-risk oxygen/sleep deprivation and reduced breathing, which damages the health of both the mouth and the body. We will advance in the battle to eradicate these causes through testing, education, and implementation.
Researchers who investigate the link between diabetes and periodontal disease have learnt that blood sugar levels and the periodontal inflammatory response appear to be related. When people consume a diet full of refined sugars, cereals, pastas, vegetable oils, and breads, it could lead to metabolic syndrome, high cholesterol and blood pressure, insulin resistance, and weight gains. This can lead to Type 2 diabetes, which creates considerable inflammation throughout the body.
So, whose responsibility is it to combat the damaging effects of high-risk blood sugar dysregulation on both the mouth and the body? Dental professionals. Dental professionals need to be the sentinels of systemic inflammation, responsible for preventing high-risk oxygen/sleep deprivation and reduced breathing, which damages the health of both the mouth and the body. We will advance in the battle to eradicate these causes through testing, education, and implementation.
Recognizing the above “Big 3” of oral-systemic inflammatory connections permits us to direct our work in the right way for those patients we serve.
That will lead us to frame a strategy of implementation as sentinels of systemic inflammation.
A STRATEGY FOR THE SENTINELS OF SYSTEMIC INFLAMMATION
Our objective is to maximize healthy conditions for each and every patient we serve through the mitigation of oral and systemic inflammation.
The “steps” for achieving this objective will be education, testing for the Big 3, and implementation.
We need to raise awareness among our patients of the risks that ensue on their overall health, from the Big 3. As the sentinels of systemic inflammation, starting a comprehensive patient education program should be the next step, with communication bolstered through thorough self-assessment questionnaires that enquire about the various conditions and symptoms that they may hold. Notify them of the diagnostics and examination processes that you administer to them, so that they can recognize their disorders, diseases, and conditions.
To take the diagnostic process further you will need testing:
If we, as dental professionals, adhere to this model of practice, we will gain progressive strategies that help improve accuracy in treatment planning and in mitigating the spread of dangerous inflammatory conditions, These can include nutritional counseling, tongue-tie release surgery, expanded periodontal protocols, expanding dental arches, and all-round collaboration with teams of dental and oral health specialists.
CONCLUSION
As oral health specialists, we should try our best to save lives! Being sentinels of oral-systemic inflammation, we understand many of the important underlying factors, we know the target and have the offensive arrows of education, testing, and implementation, and we can now passionately move forward with unwavering commitment!

| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|