Menu
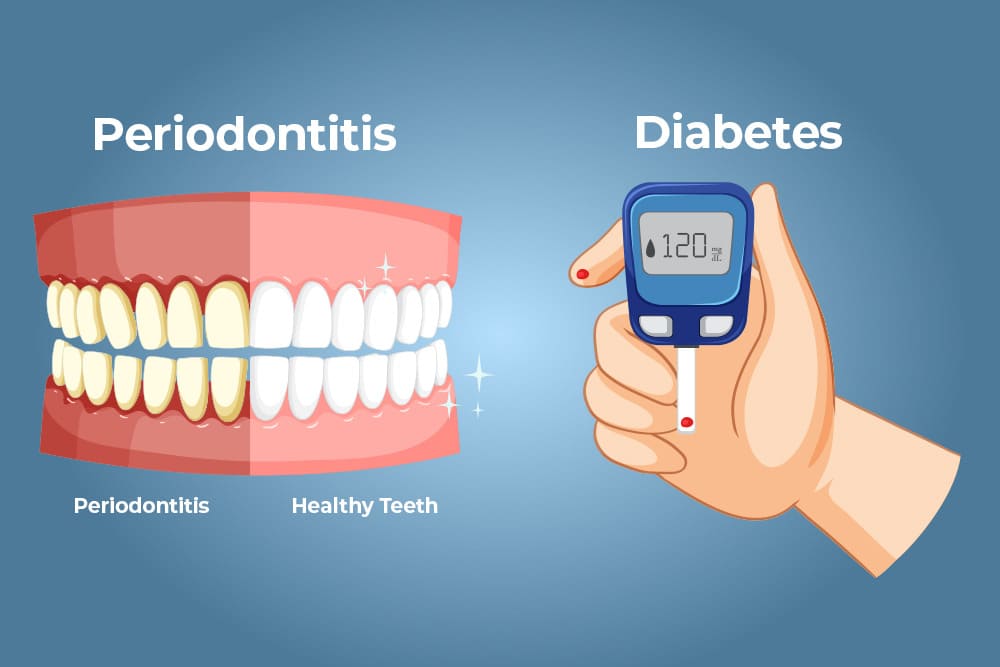
For dental professionals, the bidirectional relationship between diabetes mellitus and periodontitis is a well-established clinical reality. Systemic hyperglycemia is a significant independent risk factor for tooth loss and periodontal destruction, while periodontal inflammation can adversely affect glycemic control.
A recent systematic review and meta-analysis published in the Journal of Periodontal Research (2025) provides robust evidence on the efficacy of Non- Surgical Periodontal Therapy (NSPT) in patients with Type 2 Diabetes (T2DM). For clinicians and health-conscious patients alike, the findings reinforce a critical message: managing periodontal health is an essential component of diabetes care.
The review, which analyzed 22 studies involving over 1,500 patients, compared NSPT (subgingival instrumentation) against oral hygiene instructions (OHI) alone or no treatment.
The results were statistically significant:
A common clinical dilemma is choosing the delivery protocol. Should clinicians opt for the efficiency of Full-Mouth Disinfection (FMD) or the traditional Quadrant Scaling and Root Planing (SRP)?
The meta-analysis found no evidence of a difference between full-mouth and quadrant protocols regarding clinical outcomes. Whether the therapy is delivered in a single stage or multiple visits, the reduction in probing depths and inflammation remains comparable. This allows dental professionals to tailor the treatment plan to the patientʼs comfort, anxiety levels, and medical tolerance without compromising clinical results.
Perhaps the most clinically relevant finding regards glycemic control status. Clinicians often hesitate to perform NSPT on patients with uncontrolled diabetes due to fears of impaired healing. However, the data suggests that NSPT protocols are equally efficacious in terms of clinical outcomes for patients with uncontrolled diabetes as they are for those with good glycemic control.
Furthermore, even in patients with poor glycemic control, treatment resulted in PPD reductions comparable to those with controlled glucose levels8. This suggests that dental professionals should not delay necessary periodontal care based solely on HbA1c levels.

| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|