Shop
Shop
Showing 49–54 of 54 results
-
Trioplast 5gm
Read More Quick ViewComposition:
Triamcinolone acetonide IPNSP 0.1%w/w, Oral paste – QS.
Preservatives: Methyl paraben IP/USP0.2%wlw, Propyl paraben IP/USP0.02%w/w. Triamcinolone Acetonide is a synthetic glucocorticoid with anti-inflammatory and immunosuppressive properties.Components that improve the action of Triamcinolone:
Retention: Carboxy Methyl Cellulose: Moisture retention for faster healing
Protection: Pectin: Gelling agent with protective coating
Release: Gelatin facilitates controlled release of steroid
Clinical conditions:
Recurrent Aphthous Stomatitis (RAS)
Recurrent aphthous stomatitis (RAS), commonly known as “canker sores”, is a form of benign inflammation of the oral mucosa. Although the term “canker sores” is commonly used to describe any abnormality of the mouth, the term, strictly refers to painful oral ulcers that come and go over time.
Recurrent aphthous stomatitis affects 1 in 5 persons and usually begins in adolescence and teenage years. During an episode, it may present with 1-5 painful ulcers that last for 1 – 2 weeks. These ulcers are typically seen on the inner cheeks, inner lips, underside of the tongue, or soft palate. Just before the appearance of an ulcer, one may feel a burning sensation or a lump in the area. Ulcers may be considered minor if they are less than 1⁄2 inch and heal in less than two weeks without scarring. They are called major if they are greater than 1⁄2 inch, take longer than two weeks to heal and leave scars. Some patients may have multiple recurrent crops of small, pinpoint, painful ulcers known as herpetiform RAS (these ulcers are not related to herpes virus infection). Patients are considered to have severe RAS when they have continuous ulcers with few, if any, ulcer-free periods, regardless of the size and/ or number of lesions.
Desquamative Gingivitis
The term “desquamative” comes from the Latin word “desquamare,” meaning to scrape fish scales. Desquamation refers to the shedding of epithelium, leading to skin or mucous membrane exfoliation. Desquamative gingivitis (DG) is a clinical description of gingiva marked by severe redness, peeling, vesicles, or bullae that can result in ulcers. It affects both the free and attached gingival mucosa. DG represents a clinical manifestation of various diseases.
The most common culprits include dermatological conditions like lichen planus (LP) in 70-75% of cases, cicatricial pemphigoid (CP) in 9-14% of cases, and pemphigus vulgaris (PV) in 4-13% of cases.
Oral Submucous Fibrosis
Oral submucous fibrosis (OSMF) is a precancerous condition with chances of malignant transformation in 1.5–15% of the cases. OSMF is mainly caused by chewing betel nut, which is accelerated by addition of tobacco. Other risk factors include genetic predisposition, autoimmunity, nutritional deficiencies, human papilloma virus (HPV) infection, consumption of spicy foods, and more.
OSMF is characterized by chronic inflammation, excessive collagen deposition in the submucosal (the connective tissue below the oral mucosal epithelium) layers, local inflammation in the deep connective tissues, and degenerative changes in the muscles. OSMF patients complain of severe burning sensation in the mouth while eating spicy foods. They also experience xerostomia (dry mouth), restricted mouth opening, restricted tongue mobility, dysphagia, and many other symptoms.
Indications:
TRIOPLAST is indicated for:
- Inflammatory disorders of the mouth
- Painful ulcers, lesions of oral mucosa
- Recurrent and resistant aphthous ulcers
- Desquamative gingivitis, mucositis, and stomatitis
- Ulcerative conditions associated with Oral lichen planus, pemphigus, and pemphigoid Oral submucous fibrosis
- Non-healing ulcers of the oral mucosa, in cancer and non-cancer conditions
- Contact cheilitis
- Hemangioma
- Erythema multiforme
Contraindications:
This preparation is contraindicated in patients with a history of hypersensitivity to any of its components . Because it contains a corticosteroid, the preparation is contraindicated in the presence of fungal, viral or bacterial infections of the mouth or throat.
Directions for use:
Squeeze out about a 1/4th of an inch long ribbon of TRIOPLAST on the tip of a clean & dry finger. Apply with little pressure to the lesion until a thin film develops. Hold in position until it become sticky. The preparation should be applied at bedtime to permit steroid contact with the lesion throughout the night. Depending on the severity of symptoms, it may be necessary to apply the preparation two to four times a day, preferably after meals. Do not eat or drink for half an hour after applying TRIOPLAST.
Storage:
Store below 30’C.
Presentation:
Trioplast 0.1% oral paste is supplied in 5gm laminated tube containing 1mg of triamcinolone acetonide per gram of paste.
-
Wet Mouth 200ml New
Read More Quick ViewComposition:
Water, Glycerin, Sorbitol, Propylene Glycol, PEG 40 HCO, Poloxamer, Sodium Benzoate, Sodium CMC, Flavour, Cetylpyridinum chloride, parabens, Xylitol, Xanthan gum, Disodium hydrogen phosphate & Sodium dihydrogen Phosphate.
Mode of Action:
With their main action of hydration of oral mucosal tissues, saliva substitutes are useful agents for the palliative management of xerostomia. When used regularly, they keep oral mucosa moist and lubricated. Surface abrasion is reduced and patients can perform everyday activities of eating, sleeping, and speaking.
Causes of dry mouth:
Dry mouth can be caused by various factors, including:
1. Medications: Dry mouth is a common side effect of many prescription and nonprescription drugs. These drugs encompass those used to treat conditions such as depression, anxiety, pain, allergies, colds (such as antihistamines and decongestants), obesity, acne, epilepsy, hypertension (diuretics), diarrhea, nausea, psychotic disorders, urinary incontinence, asthma (specific bronchodilators), Parkinson’s disease, and muscle relaxants and sedatives.
2. Diseases and infections: Certain medical conditions, like Sjögren’s syndrome, HIV/AIDS, Alzheimer’s disease, diabetes, anemia, cystic fibrosis, rheumatoid arthritis, hypertension, Parkinson’s disease, stroke, and mumps, can result in dry mouth as a side effect.
3. Medical treatments: Damage to the salivary glands, responsible for saliva production, can reduce saliva output. This damage may occur due to radiation therapy to the head and neck or chemotherapy for cancer treatment.
4. Nerve damage: Nerve damage in the head and neck area, often resulting from injury or surgery, can lead to dry mouth.
5. Dehydration: Conditions causing dehydration, such as fever, excessive sweating, vomiting, diarrhea, blood loss, and burns, can contribute to dry mouth.
6. Salivary gland removal: Surgical removal of the salivary glands can lead to dry mouth.
7. Lifestyle Factors: Smoking or chewing tobacco can reduce saliva production and worsen dry mouth. Frequent mouth breathing can also be a contributing factor.Indications:
Xerostomia, Salivary dysfunction.
Directions for use:
Follow the instructions on the label. Use 15 ml using a measuring cup cum cap. Rinse thoroughly in the mouth for 30 seconds and spit out. DO NOT SWALLOW. Use a maximum of up to 5 times a day depending on individual requirements.
Presentation:
Plastic bottle of 200 ml.
-
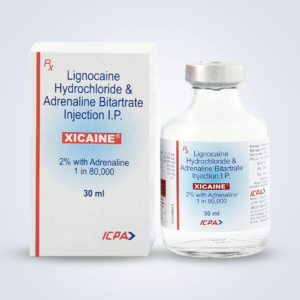
Xicaine Vials (Pack of 20..
Read More Quick ViewComposition:
Lignocaine Hydrochloride I.P. 2% Adrenaline I.P. 1:80,000
Mode of Action:
Local anesthetics reversibly block nerve transmission, when applied to a limited area of the body. They bind to the sodium channels in the nerve membrane and prevent the entry of sodium ions in response to the membrane’s depolarization. A vasoconstrictor like Adrenaline added to a local anesthetic may significantly prolong the anesthetic’s duration of action by reducing the blood flow around the injection site. This in turn may reduce the local anaesthetic’s peak plasma concentration and the risk of adverse systemic reactions.
Indications:
Local anesthesia by infiltration or nerve block injection.
Contraindications:
Xicaine is contraindicated in patients with known hypersensitivity to local anesthetic of the amide type or the presence of vasoconstrictor. Adrenaline is contraindicated in patients with arterial hypertension, coronary disease, and valvular cardiac disease.
Dosage and administration:
Adults: 2 ml is generally sufficient. 4 to 6 ml may be used if deemed necessary for prolonged procedures.
Adolescents between 14 to 17 and the elderly: The usual dose is 1.8 ml. Do not exceed 3.75 ml.
Children between 6 and 14: The usual dose is 1 to 1.5 ml. Do not exceed 2.5 ml.Caution:
Do not use under 3 years of age.
Storage:
Store in a cool dark place.
Presentation:
Vial of 30 ml (1.01 fl. oz)
-
XTAR 100gm
Read More Quick ViewComposition:
Potassium pyrophosphate, sodium pyrophosphate in a combined concentration of 5%. Plus, sodium fluoride 0.24% equivalent to 900 ppm
Understanding Pyrophosphates:
A. Tooth whitening by removal of extrinsic stains caused by tea, coffee, other beverages:
Tooth brushing is the most convenient and economical procedure to remove plaque and extrinsic stains regularly via daily home care. Using tooth-whitening toothpaste for stain removal is becoming increasingly popular.
Types of tooth-whitening toothpastes:
A. Mechanical:
Toothpastes containing abrasive agents, such as charcoal, hydrated silica, or alumina particles can remove tooth stains by mechanical abrasion. Many factors, such as the morphology, particle size, hardness, quantity of abrasive agents, and the amount of toothpaste used— significantly influence the effectiveness of stain removal.
B. Chemical:
Studies have shown that chemical agent containing whitening toothpastes can produce a similar whitening effect compared with hard abrasive toothpastes. An advantage is that the chemically acting whitening toothpastes produce lower surface roughness compared to hard abrasive particle containing whitening toothpastes.
Enzymes, antitartar compounds, and peroxides can help remove extrinsic stains. However, peroxide chemicals remain highly controversial regarding their safety and side effects.
Antitartar agents, such as pyrophosphates, are safer options commonly used as whitening agents.Pyrophosphates as the tooth whitening, stain-removal agents:
- Pyrophosphates are among the ingredients found in whitening toothpastes, which aim to remove extrinsic stains and prevent their reformation.
- Pyrophosphates tend to have strong binding affinity for enamel, dentine and tartar surfaces, and during adsorption they desorb the stain components.
- Pyrophosphates can bind with protein pellicles, preventing incoming stain-attached salivary proteins from adhering to the tooth surface.
B. Calculus formation:
Calculus formation is a common occurrence. Gingivitis and periodontitis were initially linked to the buildup of dental calculus. However, extensive in vivo research has revealed that biofilm plays a more crucial role in the development of these diseases.
Dental calculus results from the mineralization of bacterial plaque and poses a significant challenge to oral health. It exacerbates plaque and bacterial toxins accumulation and hinders their effective removal due to its rough surface. This, in turn, complicates proper hygiene maintenance and promotes further plaque buildup.
Several factors contribute to calculus formation. These factors encompass increased retention of bacterial plaque, biochemical elements like saliva and crevicular fluid composition, the characteristics of the microorganisms within the plaque, and dietary factors.
Notably, dental calculus accumulation varies widely among individuals and is not uniform across the population. Some individuals, even with good plaque control, experience rapid calculus buildup. This necessitates more frequent dental visits and complicates the management of periodontal issues.
Pyrophosphates as anti-tartar/ anti-calculus agents:
- When toothpaste containing the soluble tetra sodium/ potassium pyrophosphate is applied to the teeth and gums, a chemical bonding process occurs.
- Pyrophosphates (crystal growth inhibitor) act as chelating agent and removes calcium from the saliva to form a soluble complex that can be rinsed away with water thereby controlling new calculus buildup.
- Any calcium phosphate that has not yet bonded to teeth is attracted to the sodium pyrophosphate. When the new compound mixes with water, it is completely dissolved.
- The toothpaste cannot dissolve the tartar that has already bonded with the enamel, but it can stop future deposits from forming.
- Fluoride also inhibits the metabolism of acid-producing bacteria thereby indirectly help in tartar control in addition to controlling cavities.
Indications:
1. Individuals clinically diagnosed as heavy calculus formers, and those who want to control regular tartar build up.
2. Individuals looking to control extrinsic stain formation on teeth (eg. tea, coffee, tobacco stains, etc)Guidelines:
1. Children under 12 years of age should not use pyrophosphate-containing toothpastes .
2. XTAR should be recommended for minimum 8-12 weeks and after which doctor should evaluate the results and continue further treatmentStorage:
Keep tube capped when not in use. Store below 30°C.
Contraindications:
Known sensitivity to any of the active ingredients or excipients.
Presentation:
100 gm lamitube.
-
Younifloss
Read More Quick ViewFloss with handle for convenient flossing
Presentation :
Multitufted unwaxed floss.
-
Zingisol 15ml
Read More Quick ViewComposition:
Zinc Sulphate I.P. 2% w/v in an aqueous base.
Astringents
Astringents are chemical compounds that precipitate proteins without penetrating the cells. They affect only the superficial layer of mucosa — making the surface mechanically stronger and decreasing the exudation. The word “astringent” is derived from the Latin word adstringere, which means “to bind fast”. Astringents have relatively low cell permeability, and act generally as irritants in moderate concentrations and caustics in high concentrations.
Mode of action:
Astringents cause contraction of tissues by constricting small blood vessels, extracting water from the tissues or by precipitating proteins. Astringents are used in dentistry to cleanse and tighten the gums.
Indications:
Dentists can apply astringents to gingival tissues
1. to stop bleeding gums
2. Before taking impressions
3. Before doing Class V or root surface restorations.Directions for use:
Take 3 to 4 drops Zingisol on the fingertip and massage each quadrant 3 to 4 times a day, or as directed by the dentist or physician.
Storage:
Store in a cool, dark place. Caution: For external use only.
Presentation:
Plastic bottle of 15ml (0.5 fl.oz) with inbuilt dropper.
Quick Links
Our Products
Information
Contact us
- 216-219, Adarsh Industrial Estate, Sahar Road, Chakala, Andheri (East), Mumbai - 400099
- Fax : 28216928
- +91 22 40065305 / 40065306 / 40065307
- info@icpahealth.com

Selected Icpa Products
Click on Add to cart to add this item in cart.
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|
Selected Icpa Products
Click on Add to cart to add this item in cart.
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|