Menu
This recent expert consensus from the Journal of Clinical Periodontology (September 2025) delivers a landmark synthesis on aesthetics and patient- reported outcomes (PROs) in periodontology and implant dentistry. Drawing lessons from five systematic reviews and clinical trials, the report offers actionable, evidence-based recommendations to guide clinicians toward truly patient-centered care in soft-tissue reconstruction, gingival recession, and peri-implant therapy.
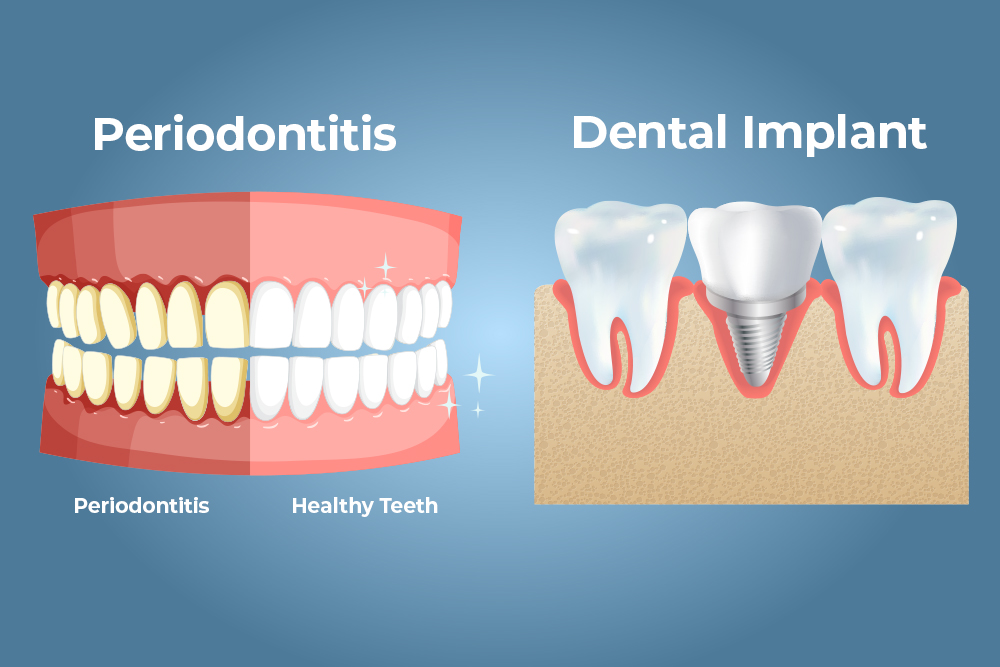
Aesthetics and patient-reported experiences have historically lagged behind clinical metrics in shaping periodontal and implant therapy decisions. Traditionally, outcome assessment revolved around clinical markers— percentage of root coverage, probing depths, or bone levels—leaving out how the patient feels or perceives the results. This consensus decisively emphasizes the need for integrating PROs and patient-reported experiences (PREs) alongside clinician-reported outcomes (CROs) to form the new gold standard.
Patient-reported outcomes directly reflect the patientʼs functional improvements, aesthetic satisfaction, and oral-health-related quality of life (OHRQoL), providing context that purely clinical endpoints canʼt capture. The expert panel calls for validated patient-reported outcome measures (PROMs), developed collaboratively with patients to set meaningful endpoints—such as the “minimally important differenceˮ that is clinically relevant to patients rather than just statistically significant.
For both single and multiple gingival recession defects, the consensus identifies the combination of coronally advanced flap (CAF) with autogenous connective tissue graft (CTG) as the standard of care for recession type 1 and 2 lesions. Both MCAF and tunnel flap techniques, supported by CTG or appropriate substitutes (such as xenogeneic collagen matrices), show strong outcomes in clinical trials. Notably, adding CTG is particularly recommended for cases with thin tissue phenotype, as it enhances both stability and aesthetic results, although it may increase procedural complexity and post-operative morbidity.
The experts stress that surgical choices should be tailored based on anatomical and patient-specific factors, including tissue phenotype, location, lesion dimensions, associated non-carious cervical lesions, and the surgeonʼs expertise. A key insight: modifying traumatic oral hygiene habits is essential for conservative management and to maintain stable results after surgery.
When it comes to immediate implant placement (IIP) in the aesthetic zone, soft- tissue augmentation (STA) with CTG helps reduce apical shifts in mucosal margins and unfavourable aesthetic outcomes, especially in high-risk scenarios (thin phenotype, minor buccal dehiscence, or high smile lines). However, existing aesthetic indices and patient satisfaction scores (such as PES, VAS, OHIP-14) often fail to sensitively capture these nuanced benefits, highlighting the pressing need for next-generation measurement tools—including AI-driven assessments and refined questionnaires.
Soft-tissue volume augmentation (STVA) during early, delayed, or late implant placement also shows clinical and aesthetic benefits—such as increased tissue thickness and improved mucosal margins—but current evidence, patient selection, and measurement tools are inadequate for strong recommendations on technique or timing.
For buccal peri-implant soft-tissue dehiscences (PSTD), surgical intervention using CAF plus CTG achieves positive aesthetic outcomes and high patient satisfaction with minimal morbidity, though coverage is more challenging around implants than natural teeth. Modifying prostheses may help improve soft-tissue adaptation in select cases. The consensus underscores the need for multidisciplinary inputs, especially where implant positioning or restorative design hinders ideal results.
The experts make a compelling case for harmonizing CROs, PREs, and PROs as co-equal pillars of evidence-based medicine in periodontology and implant dentistry. This means not only measuring what can be easily observed or quantified clinically but also rigorously capturing what patients value—function, aesthetics, comfort, and quality of life—across diverse scenarios and populations.
Clinicians, researchers, and industry are challenged to design and validate responsive PROMs, improve transparency in outcomes reporting (CONSORT non-pharmacological extension), invest in sensitive assessment methods, and embrace co-production with patients for future research. Only then can periodontology and implant dentistry deliver on the promise of personalized, meaningful care—where every intervention is measured not just by numbers, but by its impact on real lives.
These advances are set to transform clinical decision-making, research standards, and patient satisfaction in periodontal and implant therapy, with robust scientific evidence and patient experience firmly at the center of care.
Tonetti M, Sanz M, Cairo F, Nart J, Chapple I, et al. Aesthetics and Patient- Reported Outcomes in Periodontology and Implant Dentistry: Consensus Report. J Clin Periodontol. 2025 Sep;52(9):1222-1244. doi: 10.1111/jcpe.14182. Epub 2025 Jun 10. PMID: 40495112; PMCID: PMC12377961.

| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|