Menu
Periodontitis is more than just a dental issue. It is a chronic inflammatory non-communicable disease (NCD) that leads to the progressive destruction of the supporting structures of teeth, including the alveolar bone. Clinically, it manifests as periodontal pockets, bleeding on probing, and, if left untreated, tooth loss.
The disease begins with the accumulation of microbial biofilm around the gum margin. This triggers a host immune-inflammatory response which, in turn, fuels further microbial imbalance (biofilm dysbiosis). The result is a vicious cycle of inflammation and tissue destruction that undermines oral and general health alike.
The management of periodontitis follows a structured approach:
1. Step 1: Supragingival biofilm control and risk factor modification (e.g., smoking cessation).
2. Step 2: Subgingival instrumentation with or without adjunctive therapies.
3. Step 3: Surgical approaches for severe cases.
4. Supportive Periodontal Care (SPC): Long-term secondary prevention— professional cleaning 2–3 times a year and tailored patient oral hygiene practices.
This tiered approach ensures that most mild and moderate cases can be managed non-surgically, while severe forms receive advanced interventions.
The recognition of periodontitis as more than a dental problem is not new.
Both workshops underscored the essential role of collaboration between family doctors and oral healthcare professionals (OHPs) in managing these co-morbid conditions.
Building on these foundations, a third EFP Focused Workshop was convened to define best practices for integrating oral and general healthcare. This workshop placed special emphasis on:
The consensus from this workshop represents the most comprehensive effort yet to bridge dentistry and medicine for better NCD management.
The third workshop was designed with two clear goals:
Objectives
Methods
This structured approach ensured that the final recommendations were not just expert opinions, but carefully reviewed and evidence-backed guidance.
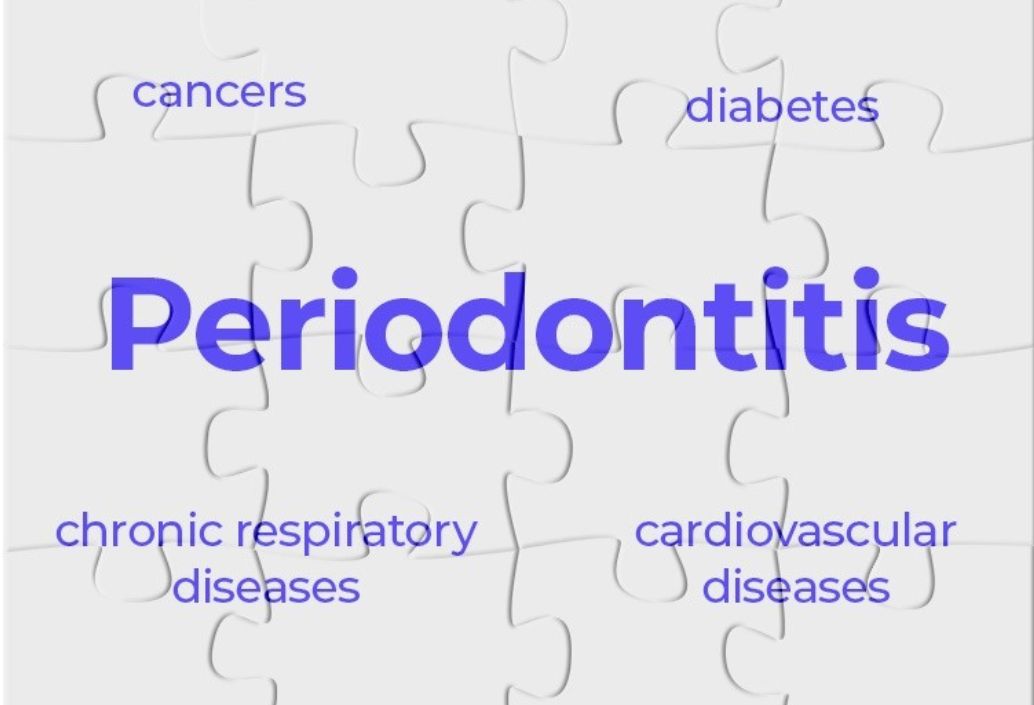
Strong evidence now confirms that periodontitis is not confined to the oral cavity— it is independently associated with several major non-communicable diseases, including:

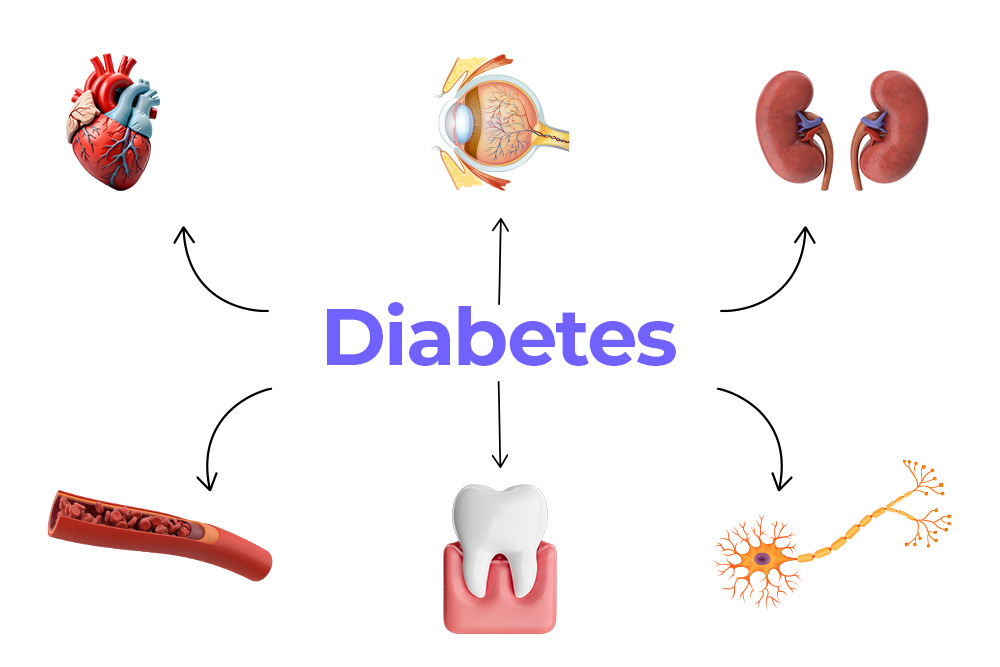
Encouragingly, treatment of periodontitis has been linked to improvements in systemic health outcomes, such as better glycaemic control in diabetes and reductions in markers of cardiovascular risk.
However, important evidence gaps remain, particularly around causality, long-term outcomes, and optimal models of collaborative care. This underlines the need for stronger integration between medical and dental practice.
Both oral health professionals (OHPs) and family doctors have a central role to play. Practical strategies should include:
Closer collaboration is critical. Joint efforts between OHPs, family doctors, and healthcare funders can improve early detection, prevention, and management of NCDs. To support this, evidence-based information on periodontal–systemic links must be made widely available—not just to clinicians, but also to patients, policymakers, and the broader public.
The consensus is clear: oral health care professionals (OHPs) and family doctors must work together.
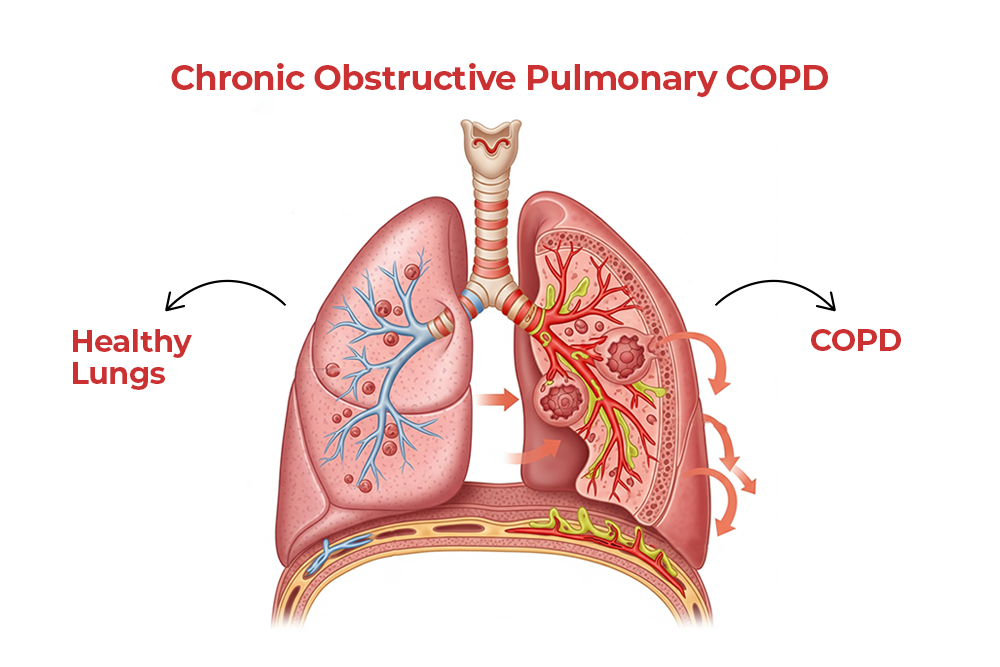
1. Periodontitis is linked with cardiovascular disease, diabetes, COPD, obstructive sleep apnoea, and COVID-19 complications.
2. Effective periodontal treatment improves systemic outcomes, particularly in diabetes and cardiovascular health.
3. Closer collaboration between oral health professionals and family doctors is critical for early detection and management of NCDs.
4. Evidence-based information must reach not only professionals but also patients, policymakers, and the wider public.
Periodontitis is not just a dental condition—it is a public health priority with far-reaching consequences. By bridging the gap between dentistry and general medicine, healthcare professionals can better manage NCDs, reduce inequalities, and promote healthier lives.
The time has come to move beyond siloed care. Oral health and general health are inseparable, and periodontitis is the bridge that reminds us of this truth.
Herrera D, Sanz M, Shapira L, Brotons C, Chapple I, Frese T, Graziani F, Hobbs FDR, Huck O, Hummers E, Jepsen S, Kravtchenko O, Madianos P, Molina A, Ungan M, Vilaseca J, Windak A, Vinker S. Periodontal diseases and cardiovascular diseases,
diabetes, and respiratory diseases: Summary of the consensus report by the European Federation of Periodontology and WONCA Europe. Eur J Gen Pract. 2024 Dec;30(1):2320120. doi: 10.1080/13814788.2024.2320120. Epub 2024 Mar 21. PMID: 38511739; PMCID: PMC10962307.

| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|
| PRODUCTS | QTY | PRICE | VALUE in INR |
|---|